Posted February 1, 2005: by Bill Sardi
It’s a stealth bacterium, undetectable by most modern laboratory methods.
It has infected more than 40% of dairy herds in the US and reduced their milk production by 4 percent. It’s now positively linked to inflammatory bowel disease (known as Crohn’s disease) that infects 500,000 Americans and is a probable cause of irritable bowel syndrome (chronic diarrhea, also known as colitis) that afflicts many more.
The germ involved is mycobacterium paratuberculosis (PARA-TB), a stealth bacterium that emanates from cattle herds and eludes detection and destruction.
Due to changes over many years in the feeding of cattle (they are now grain fed rather than grass fed), the digestive system of milk cows is less acidic and 40% or more of dairy herds are infected with PARA-TB, as well as many other forms of bacteria such as E. coli, Salmonella and Campylobacter. The overall bacteria load of raw milk is much higher than decades ago.
PARA-TB is shed from the cows, resides in raw milk, and resists Pasteurization. The most recent study published in the Journal of Food Protection shows nearly 3 percent of retail milk cartons obtained from California, Minnesota and Wisconsin harbor PARA-TB (possibly more than half of Pasteurized milk may harbor PARA-TB in summer months). [J Food Protection, 68: 966-72, 2005]
Other published studies also confirm that PARA-TB escapes Pasteurization and is harbored in retail milk cartons. In a test of retail milk samples conducted in Ontario, Canada, 15% (110 of 710) were contaminated with mycobacterium paratuberculosis. [Journal Dairy Science 85: 3198-3205, 2002] Up to 25% of milk cartons in England were found to contain DNA from PARA-TB. [Applied Environmental Microbiology 62: 3446-52, 1996]
“How is Crohn’s transmitted to humans? The shocking answer is through that most sacrosanct of beverages—milk.
[LA Times, Sept. 18, 2000]
It should come as no surprise that Crohn’s disease rates are highest in countries where milk consumption is high, except where milk is traditionally boiled prior to consumption. Examine the following chart. The low-milk drinking countries have almost non-existent rates of Crohn’s disease.
|
Per Capita Consumption (kg) of Milk and Milk Products in Various Countries, 2000 data., |
||||
|
Country |
Fluid Milk Kilograms |
Cheeses |
Incidence of Crohn’s |
Reference data |
|
Ireland 1 |
163 |
7.0 |
5.9 |
Dublin 1996 |
|
Sweden 2 |
157 |
16.6 |
4.9 |
2003 |
|
UK 3 |
117 |
9.7 |
10.1-11.1 |
1991-92 |
|
Netherlands 4 |
101 |
14.6 |
6.9 |
1998 |
|
USA 5 |
97 |
14.0 |
4.56 |
Wisconsin 2003 |
|
Canada 6 |
90 |
11.6 |
14.6 |
Manitoba 1994-95 |
|
France 7 |
68 |
23.2 |
4.9 |
1994 |
|
Germany 8 |
63 |
12.8 |
5.1 |
Cologne 1986 |
|
Italy 9 |
63 |
20.6 |
2.8 |
Florence 1996 |
|
Japan 10 |
39 |
1.8 |
1.86 |
1988 |
|
China 11 |
2 |
– |
1.00 |
2004 Hong Kong |
| 1- Gut 39: 690, 1996 2- Gut. 2003 Oct;52:1432-4 3- Eur J Gastroenterol Hepatol. 1998 Dec;10:1007-12. 4- Dis Colon Rectum 41:33-40, 1998 5- J Pediatrics. 2003 Oct;143:525-31, 2003 6- Crohn’s and Colitis Foundation, Canada 7- Gut. 1994 Oct;35:1433-8 8- Med Klin (Munich). 1993 Sep 15;88:516-9 9- Scand J Gastroenterol. 1996 Sep;31:892-9 10- Gastroenterol Jpn. 1988 Oct;23:521-6. 11- Inflammatory Bowel Diseases. 10:646-651, September 2004 | ||||
Not only has PARA-TB been found in Crohn’s disease by five investigative groups in different countries, but Crohn’s patients, and cattle that have a similar malady called Johne’s disease, have antibodies which cross react with antigens from PARA-TB. Stealth Pathogens, CRC Press 2001]
The occurrence of Crohn’s disease appears to rise in geographical areas, which makes one think that there is an environmental contaminant. [Archives Neurology 61: 1057-60, 2004]
Mycobacterium avium subspecies paratuberculosis, causes inflammatory bowel disease (Johne’s disease) in cattle, sheep, deer, bison, monkeys and chimpanzees. “The evidence to support PARA-TB infection as a cause of human Crohn’s disease is mounting.” [Alimentary Pharmacol Therapy 15: 337-46, 2001]
Crohn’s is a punishing disease. About 25-45% of patients with Crohn’s undergo surgery within 3 years of diagnosis. For many, Crohn’s is a slow death sentence. Mortality over time is about 5 percent. [Gastroenterol Clin Biology 12:1233-9, 2004] Almost half of the women that have Crohn’s disease report pain during intercourse and approximately forty percent have ovarian cysts. Imagine the frustration experienced by Crohn’s sufferers as they try to alert the rest of the world, only to be closeted by the news media and public health authorities.
The dairy industry keeps denying there is a problem, saying their cows are not sick, but cows, like humans, can be infected without exhibiting symptoms. The US Department of Agriculture refuses to test retail milk samples for PARA-TB. Dairymen and public health authorities say they are withholding any action till human disease is positively linked with PARA-TB infection. How much more evidence is needed?
While thousands of milk drinkers are swallowing down PARA-TB laden milk, the experts continue to debate. The reason for the foot-dragging is that PARA-TB is not easily detected by conventional microscopic methods, and it may take a year to culture and grow to be detected in milk samples. Only sophisticated DNA testing can repeatedly detect PARA-TB in Crohn’s patients. It was only when doctors began prescribing to Crohn’s patients the few antibiotics known to kill lung TB, with notable remissions, that it became apparent PARA-TB is the likely cause of inflammatory bowel disease.
Dairymen and public health authorities may be more attuned to protecting sales of dairy products than human health. At risk is $30 billion in annual sales of milk. Cheese also harbors PARA-TB but hasn’t been widely tested. Cattle herds for meat are infected also.
This report is not ground breaking. The link between PARA-TB and Crohn’s was reported in the Saturday Evening Post in 2004, the Los Angeles Times in 2000 and the Cleveland Free Times in 1999. An article in the September, 2000 issue of the Los Angeles Times said: “How is Crohn’s transmitted to humans? The shocking answer is through that most sacrosanct of beverages—milk.” [LA Times, Sept. 18, 2000]
Crohn’s disease groups along with the National Milk Producers Federation requested federal assitance in 2001 to clean up the animal herds, but the use of antibiotics would spawn drug-resistant forms of PARA-TB that could literally wipe out cattle herds and human populations, and massive slaughter of so many infected animals would produce an economic disaster. The only real long-term answer is to return to grass feeding of cattle herds. Some cattlemen already offer meat from grass-fed animals. Author Jo Robinson provides assistance in finding grass-fed animal products at www.eatwild.com. Also, her book, Pasture Perfect, is a worthwhile read.
It’s time to face up to a public health catastrophe of horrendous proportions. Most Americans should consider they may already harbor the PARA-TB bacterium in their body. Crohn’s and colitis patients should go to their doctors and demand a course of antibiotic therapy, and refrain from milk products. Various methods of keeping PARA-TB at bay, by boosting natural immunity, are strongly advised, and described later in this report. Use of boiled milk, or yogurt or tapioca, which are boiled during processing, may serve as safe alternatives to Pasteurized milk.
Paratuberculosis has been shown to survive Pasteurization in raw milk samples. [Applied Environmental Microbiology 71: 1785-89, 2005] Viable PARA-TB has been found in milk pasteurized at 72 degrees Celsius for 15 seconds. [Applied Environmental Microbiology 71: 1785-89, 2005]
When large numbers of PARA-TB are present in raw milk, it is more difficult to kill all organisms by Pasteurization. [Applied Environmental Microbiology 62: 631-36, 1996]
There may also be a glitch in the Pasteurization process. It has been shown that raw milk needs to be Pasteurized in a turbulent flow to achieve complete inactivation of bacteria. [National Animal Disease Center, USDA, 5th International Colloquim on Paratuberculosis, Oct. 3, 1996]
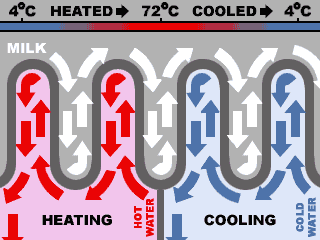
Organic milk is not safer, just maybe less pesticides. Ultra-pasteurized milk is not likely to be safer either. Standard Pasteurization raises milk temperature to 161 degrees Farenheit for 12 seconds. Longer time rather than higher temperature appears to be more important. Ultra-Pasteurization (280 degrees Farenheit for 2 seconds), promoted by some organic dairies because it extends shelf life, may harbor more PARA-TB and other bacteria. Some tests show a 25-second Pasteurization cycle would kill off nearly all bacteria. [Letters Applied Microbiology 28: 461-65, 1999] Irradiation has been shown to destroy the paratuberculosis bacterium in milk and could be an alternative to heat pasteurization. [Dairy Herd Management, September 2001]
The question will arise, what about raw unpasteurized milk, which many claim is healthy? Advocates for raw unpasteurized milk probably refer to cow’s milk produced from grass-fed animals with low bacterial counts. Some cows that produce raw milk reside in pastures with alkaline soil and low iron levels and thus low PARA-TB levels. So they are not shedding much PARA-TB. The safety of raw milk depends upon soil conditions and feeding practices.
In the 1930s and 1940s Christmas Seals were sold to fight tuberculosis. People were also encouraged to drink milk to prevent and cure tuberculosis.
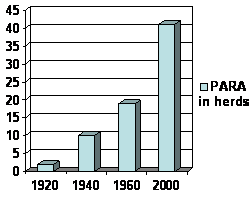
Crohn’s disease wasn’t widely reported till the 1920s. This correlates with the rapid rise in PARA-TB infection in cattle herds since that date. Obviously, something happened in the way dairy herds were handled to promote the overgrowth of this bacterium in cattle. Infectious bacteria abound in cattle because of the practice of grain feeding. Grass fed animals do not harbor nearly as much E. coli, Salmonella or mycobacteria. In the US, cattle owners would rather fatten their herds on grain to raise profit margins, and throw the burden of killing germs on the consumer, who is blamed for undercooking meat if food borne infection occurs.
A tacit admission to the problem of human PARA-TB infection from contaminated milk occurred in 2000 when the National Milk Producers Federation requested $1.3 billion from Congress to cull dairy herds of infected animals. [Scripps Howard News Service, May 29, 2000]
Cheryl Miller, Co-executive Director of the Paratuberculosis Awareness & Research Association (PARA) says: “The dairy industry has been well aware of the PARA-TB-Crohn’s connection for decades. Instead of investing in research to solve the problem, they have chosen instead to launch clever marketing campaigns aimed at children–with the full knowledge that MAP may be causing Crohn’s in those children. People’s lives are ruined by this devastating disease. Children are suffering.” (For more information visit the Paratuberculosis Awareness & Research Association (PARA) website at: www.crohns.org )
John Hermon-Taylor, professor of surgery at St. George’s Hospital Medical School in London says “I am absolutely certain that some strains of paratuberculosis can be pathogenic for humans and cause Crohn’s disease.”
A study by the Ministry of Agriculture in Britain found that researchers could grow PARA-TB from at least 3% of samples of commercial pasteurized milk, Hermon-Taylor said. “It confirms, as sure as God made little green apples, that retail milk in Britain is a definite source of human exposure to these bugs,” he added. [Los Angeles Times, Monday, September 18, 2000]

Hermon-Taylor indicates PARA-TB is more robust than TB, can evade recognition by the human immune system, probably causes malfunction of the immune system, is resistant to standard antibiotic drugs, and can persist for years without causing disease. While meat is likely infected, the greatest risk to human populations is conveyed in retail milk. PARA-TB can resist heat and survive Pasteurization. Antibiotic drugs specifically effective against PARA-TB such as rifabutin and clarithromycin may eradicate the disease. “The problems causes by PARA-TB constitute a public health issue of tragic proportions for which a range of remedial measures are urgently needed.” New drugs are needed. [Canadian Journal Gastroenterology 14: 521-39, 2000] In the view of Dr. Hermon-Taylor, “There is overwhelming evidence that we are sitting on a public health disaster of tragic proportions.” [Chemist & Druggist 29:11, 2000]
Is the dairy industry aware of the problem? A study published in a 2002 volume of the Journal of Dairy Science concedes paratuberculosis in milk “is a potential source of human exposure to this organism.” [J Dairy Science 85:3198-205, 2002]
An article in Milk Science International entitled “Is Mycobacterium paratuberculosis a possible agent in Crohn’s Disease?” warns that “the present state of knowledge is… potentially catastrophic for the dairy industry…” [Milk Science International 52:311-6, 1997]
Proof that paratuberculosis infection (called Johne’s disease in cattle) causes Crohn’s disease in humans would “create a backlash that would devastate dairy product and meat sales,” so said an article published in Dairy Today in 2001.
In 1998 the US Animal Health Association drafted a resolution that urged US Department of Agriculture to fund studies to determine if paratuberculosis can be found in retail milk. A subsequent debate ensued at a meeting of the US Animal Health Association, and here is a verbal exchange that took place at their meeting:
Conclusion: This resolution was voted down by an overwhelming majority. [US Animal Health Association, October 15, 1998]
In 2001 the Food Standards Agency (FSA) in Britain demanded action by the dairy industry to find ways to treat milk so resistant bacteria would not survive Pasteurization. [London Daily Mail June 20, 2001]The Dairy Council insisted that milk is still perfectly safe to drink and that the precautionary measures should not generate alarm. But advisors to the FSA decided the risk is sufficient to require the dairy industry to introduce new safeguards. The milk industry in Britain is reported to have voluntarily increased Pasteurization time in 1999 from 15 seconds to 25 seconds as a precautionary measure.
Crohn’s diseases arises more often in the second and third decade of life, but the initial infection may have occurred in the “milk drinking years” of childhood, and the slow-growing PARA-TB bacterium eventually grew to “disease proportions” in young adulthood. Humans must be alerted that infection most likely begins in childhood and emanates many decades later in life.
Copyright 2005 Bill Sardi All rights reserved. Not for posting on other websites.
Addendum: For the sake of brevity, the following data didn’t make it into the above report. But because denial of a link between Crohn’s disease and milk is anticipated from dairy industry representatives, the following corroborative information is provided. If you still find it difficult to believe an infectious bacterium may already have taken up residence in your body via consumption of contaminated milk, consider this additional evidence:
It has been known since 1936 that raw milk is the chief means by which milk-borne tuberculosis is transmitted to humans. [Journal Dairy Science 19: 435, 1936]
Milk producers and health authorities keep hiding behind the fact that live PARA-TB is not always cultured from retail milk samples, but PARA-TB may take up to a year to culture (grow) to detectable levels. [Journal Dairy Science 85: 3198-3205, 2002]
In Czechoslovakia, researchers examined milk in cartons that were processed according to European Union standards. They report that dairy cows infected with paratuberculosis, but show no symptoms of infection, are transmitting paratuberculosis to their milk and about 2% of pasteurized milk in cartons still harbor this bacterium. The report says “humans are being exposed to this chronic pathogen by this route.” [Applied Environmental Microbiology 71: 1210-14, 2005]
Researchers in Manitoba, Canada, could not find significant differences in PARA-TB levels in Crohn’s disease patients and healthy people. They also claimed that Crohn’s disease patients were less likely to have consumed unpasteurized milk, but this assumes Pasteurized milk harbors no bacteria. Because of the stealth nature of PARA-TB, which cannot be easily cultured from blood samples, studies like these may only delay the inevitable. Manitoba residents have much higher blood levels of PARA-TB than people living in Wisconsin or Denmark, areas where dairy consumption is high. Manitoba also has a very high rate of Crohn’s disease. [J Clinical Microbiology 42: 1129-35, 2004]
Some researchers argue if Crohn’s disease is caused by a bacterial infection then why doesn’t antibiotic therapy resolve the symptoms of the disease? But many studies utilized antibiotics that are ineffective against PARA-TB. Only a narrow number of antibiotics effectively kill TB and PARA-TB. Macrolide antibiotics do resolve the infection, so a cure is possible. [Lancet Infectious Disease 4: 136-37, 2003]
Copyright 2005 Bill Sardi All rights reserved. Not for posting on other websites.
Posted in Diet ; No Comments »
You must be logged in to post a comment.
11
17
52
95
14
24
237
6
56
43
10
116
15
66
105