Posted May 19, 2011: by Bill Sardi
While cardiologists cast a blind eye at potential liver and muscle side effects induced by statin cholesterol-lowering drugs, natural health advocates suggest coenzyme Q10 supplementation to avoid the potential side effects of muscle degeneration (myopathy) associated with these drugs. In fact, coenzyme Q10 supplementation (100 mg/day) has been shown to reduce the severity of muscle pain among statin drug users by 40%. However, there is more to this story than C0-Q10.
For some time now it has been noted in the medical literature that the pattern of side effects associated with statin drugs resembles selenium deficiency. Statin drugs have a negative effect upon selenium proteins which does seem to explain many of the enigmatic effects of statin drugs. The underlying biochemical mechanisms for this are now well described.
Another fact that should also be called to attention is that reduced production of selenium-linked proteins in the body is directly related to genetic muscle disease, similar to myopathy produced by statin drugs.
Researchers in Germany now clearly show that statin drugs commonly reduce a selenium-activated antioxidant which causes abnormalities in muscle tissue and liver and results in symptoms of muscle pain and elevated liver enzymes.
While advocates for statin drugs point to very low side effect rates (less than 1%), in fact approximately 20% of patients treated with statins experience elevated liver enzymes and high-dose statin therapy results in muscle pain among 10% of patients.
The primary mechanism producing these liver abnormalities is now identified as statin drug reduction of a protective antioxidant enzyme called glutathione peroxidase. This antioxidant is produced naturally within the body from precursors vitamin E and the trace mineral selenium. Statin cholesterol-lowering drugs have also repeatedly been shown to decrease blood levels of vitamin E.
All statin drugs reduce glutathione peroxidase activity in liver cells at typically prescribed doses. Liver cells then become more vulnerable to threats from other toxins. These abnormalities are reversed by the provision of selenium.
The protective role of selenium in heart disease goes underappreciated. It is now recognized that it is oxidized (hardened) cholesterol deposits that present problems in the circulatory system and selenium produces an anti-oxidant enzyme called glutathione peroxidase which inhibits oxidation of cholesterol, particularly LDL cholesterol. In fact, the human body attempts to up-regulate the production of glutathione peroxidase as circulating cholesterol levels rise in an attempt to prevent oxidized cholesterol.
In rodents, the provision of supplemental selenium diminishes oxidation among cholesterol-fed animals.
However, this subject gets a bit confusing when studies show that higher blood concentrations of selenium are associated with elevated levels of total and LDL cholesterol in humans. One interpretation of this finding is that selenium protects the liver, which is where most cholesterol is produced, and when the liver works better, cholesterol levels rise. If selenium activated glutathione peroxidase minimizes oxidized cholesterol, rendering it harmless, why be so over-concerned about cholesterol numbers?
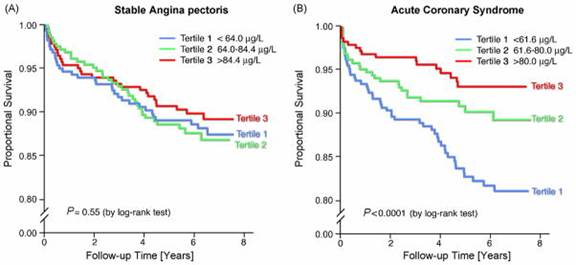
The bottom line is to prevent mortality from heart disease. Indeed, among acute coronary syndrome patients, circulating selenium levels have been measured and patients with the highest levels of selenium exhibited a relative 62% reduction in cardiac death. The concentration of selenium in the blood stream is related to future cardiovascular-related death among these acute patients.
Decades after the first cholesterol-lowering drug was introduced, recent studies concede that “optimal target levels for cholesterol and blood pressure are not clear yet.” This is difficult to believe with the major thrust of modern preventive medicine being cholesterol reduction.
Cholesterol levels gradually rise from age 20 to 65, but decline slightly thereafter in men and level off in women. Elevated cholesterol is common among senior adults – – 61% of women between age 65 and 74 have total cholesterol levels over 240. Increased blood cholesterol levels at an advanced age are less of a risk factor. In fact, by age 75 the predictive value of cholesterol for a future heart attack has disappeared. Researchers even concede that “high cholesterol is associated with longevity.” The use of cholesterol-lowering drugs among 80 and 90-year old adults with no established coronary heart disease should be called into question.
Albeit, a study of Japanese centenarians found they had higher total cholesterol are associated with better physical and brain function. This has been called the “centenarian paradox.” Maybe it would be better just to prescribe selenium and leave the statin drugs in the pharmacy closet, particularly for the most aged.
The rationale for using statin drugs is that they save lives, so the liver toxicity is tolerated. However, Harvard professor John Abramson examined whether statin drugs in fact lower mortality rates for coronary heart disease. Dr. Abramson examined the top ten studies involving statin drugs and while these drugs did reduce circulating levels of cholesterol, they did not significantly lower coronary artery disease mortality rates. This is all very well documented in the medical literature and certainly must be known by health authorities, namely the Food & Drug Administration.
Statin drugs are the second major drug class, approved by the FDA, which induce known liver toxicity. The other major drug class that causes liver toxicity is the pain reliever acetaminophen (Tylenol). Acetaminophen toxicity causes 450 deaths and 56,000 emergency-room visits a year. A sulfur compound, N-acetyl cysteine (NAC), available as a dietary supplement, is the antidote for acetaminophen poisoning. However, selenium is also a strong antidote for acetaminophen poisoning as well.
Shortages of selenium and vitamin E increase the lethality of acetaminophen in mice. Death of these animals does not involve liver toxicity, so measurement of liver enzymes may not be helpful in detecting the deadly threat posed by this pain reliever. PMID: Physicians must not rely upon liver enzyme studies alone to determine the mortal threat posed by acetaminophen.
When laboratory rats are pre-treated with selenium prior to being given acetaminophen, drug toxic effects upon the liver are decreased. Selenium appears to exert its liver protective properties by enhanced production of glucuronate, a detoxification molecule produced in the liver, rather than by up-regulation of glutathione peroxidase. While it has been recommended that NAC be added to acetaminophen tablets to prevent toxic side effects, the FDA has not demanded such an action and drug companies have largely ignored this simple solution. Ditto for selenium. An estimated 32 million Americans take statin drugs. An estimated 50 million Americans take acetaminophen products annually.
The superiority of selenium organically bound to an array of proteins, as provided in Seleno Excell® ( http://www.cypsystems.com/products/seleno.html ), has recently been validated. Organically bound selenium (selenocysteine, selenomethione, etc) rather than inorganic (selenite, selenate) has been found to activate more genes. Also, organically bound forms of selenium do not pose the risk of becoming pro-oxidants that can damage DNA as produced by selenite or selenate.
© 2011, Bill Sardi, Knowledge of Health, Inc. Not for posting on other websites.
Posted in Dietary Supplements, Minerals, Modern Medicine ; No Comments »
You must be logged in to post a comment.
11
17
52
95
14
24
237
6
56
43
10
116
15
66
105