Posted August 23, 2011: by Bill Sardi
The announcement was overshadowed by the gloom and doom surrounding the world economies. While the stock market was tumbling and the price of gold soaring, University of Pennsylvania researchers were reporting the first full remissions from leukemia (cancer of the blood) by activation of patients’ own white blood cells (T-cells, produced in the thymus gland).
The announcement came on the heels of a newly reported survey showing cancer is the most feared life-threatening disease over Alzheimer’s, stroke or heart attack.
Sluggish white blood cells (aka lymphocytes) were extracted from the patients’ own blood and genetically reprogrammed to attack roaming cancer cells. The full scientific report can be viewed here.
A number of prior attempts to employ genetically engineered T-cells had been unsuccessful. But the recognition that a type of T-cell (CD8) has a high capability to recognize, intercept and destroy malignant cells, has been the impetus that led to this most recent discovery.
The experiment, using live patients not lab rats, involved removal of patients’ white blood cells, sending them to a genetic laboratory for “reprogramming,” and then injecting them back into patients using a viral vector (carrier) that delivers an antibody-like protein called a chimeric antigen receptor (CAR), which is expressed (switched on) on the surface of T-cells and designed to target and bind to proteins called CD19. This all sounds so very complicated, and it is. This technology was 20 years in the making. The T-cells started to express CAR that focus their cancer-killing activity on cells that express CD19 protein which includes chronic lymphocytic leukemia tumor cells. More remarkably, these engineered T-cells replicated and continued making clones that prolonged the cancer-killing effect. A bigger army of T-cells was created, enough to kill off two pounds of cancer cells per patient.
The idea of boosting immunity to fight cancer has long been dismissed in favor of toxic chemotherapy drugs and is only now experiencing a revival. The idea of genetically activating T-cells to target cancer cells in this same manner was being discussed at least over a decade ago.
Till now, this approach was limited by the compromised immune system of cancer patients and inability to get intravenously administered T-cells to survive and replicate.
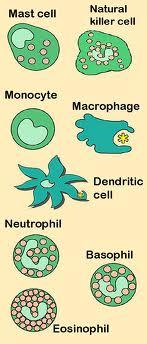
Another recent discovery suggests a similar approach to destroying cancer cells by infusing a completely different type of activated white blood cell from healthy donors into cancer patients. In this instance, rather than injecting activated T-cells, neutrophils (also known as polymorphonuclear granulocytes) are injected.
Neutrophils represent 50-70% of total white blood cell volume and are the first responders to infection or malignancy. Because neutrophils are short-lived white blood cells, they have been hastily dismissed as tumor fighters and, and as you will learn below, neutrophils may actually under some circumstances promote cancer.
The idea of employing neutrophils was initially spawned from the discovery of a strain of mice that were found to be cancer-proof. That discovery was made by Zheng Cui at Wake-Forest University in 1999 and first reported in 2003.
In a subsequent study, Dr. Cui found cancer cell-killing neutrophils could be harvested from cancer-resistant animals and injected into tumor-laden mice with the same curative effect.
Dr. Cui was curious to investigate whether this same cancer-resistant phenomenon was present in humans as in a strain of laboratory mice. He began to draw blood samples from his students to determine if any of them had active neutrophils that pursued tumor cells with the same vigor as seen among the cancer-proof mice. Surprisingly, they did.
While Dr. Cui has been obtaining blood samples from his students and analyzing them for their ability to kill cancer cells for a few years now, only recently has Dr. Cui published his human study. Blood samples from 22 patients with cancer and 25 healthy patients were analyzed for their cancer killing activity. Cancer cell killing was lower among cancer patients than healthy subjects. Strikingly, females with low cancer killing activity were 385% more likely to develop cancer than males.
But while Dr. Cui now documents his findings in humans for the first time in a published report, his paper fails to reveal what he said orally a couple of years back. In an online lecture videotaped and archived online Dr. Cui talked about his shock-wave announcement of the existence of cancer-proof mice and later cancer-proof humans.
In Dr. Cui’s lecture he mentions the work of Dr. Chester Southam at the Sloan Kettering Cancer Insitute who injected cancer cells into willing volunteers in 1957, and only a couple of them actually died from this injection. So the evidence that the human immune system can overcome cancer has been known for more than 50 years.
This boldly says the human immune system IS capable of overcoming cancer even when lethal doses of cancer cells are intentionally injected. But this fact has been ignored or dismissed by cancer researchers. Will they ever let immunotherapy get out of the starting gate?
Click to view video of neutrophil siding up to cancer cell and blowing it up with a burst of free radicals:
[hana-flv-player
video=”http://knowledgeofhealth.com/wp-content/uploads/2011/08/killingCancer.flv”
width=”320″
height=”240″
description=”neutrophil siding up to cancer cell and blowing it up with a burst of free radicals”
clickurl=”http://knowledgeofhealth.com”
clicktarget=”_blank”
player=”4″
autoplay=”false”
loop=”true”
autorewind=”true”
/]
Dr. Cui added that cancer resistance noted in humans was only observed in summer months and wore off around Thanksgiving and lasted for six months. “During the entire winter season nobody has cancer resistance,” said Dr. Cui. And cancer patients have almost no neutrophil activity during these months either, he said.
Cancer typically is seasonal, peaking in winter and abating in summer. Cancer patients survive longer when first diagnosed in summer and when they vacation in sunnier climates. Obvious, this all points directly towards vitamin D, the sunshine vitamin, as the major controlling agent in cancer.
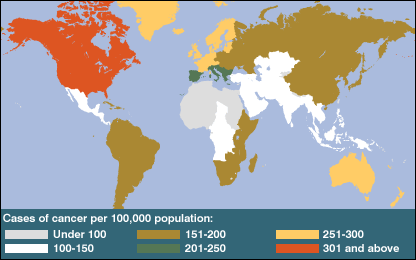
It’s not like Dr. Cui doesn’t know about vitamin D. During his lecture he shows a slide of the world revealing there is no cancer season (or even a flu season) in lands close to the equator, where sun intensity is the highest. “This is like a vitamin D risk curve,” says Dr. Cui, as he notes the seasonal pattern of cancer. But he says “this would be too simple” if vitamin D cured cancer.
Dr. Cui reveals that a number of potential investors had inquired about new technologies that could be developed. He said that his idea of taking neutrophils out of healthy adults and infusing them into cancer patients was ready for a trial and the FDA had been petitioned to approve a treatment protocol. But the trial never commenced.
Why would Dr. Cui take the more difficult course, wait for summer to withdraw blood samples with activated cancer-killing neutrophils and then infuse them into cancer patients when possibly vitamin D pills are all that is needed?
As he said, that would be too simple. There would be no business, no profits, maybe no patents. So that is the end game in cancer, to strike it rich, not cure patients. In this perverse system, only expensive cures are tested. Simple more economical approaches are shunned or ignored, like vitamin D, which activates the very neutrophils that Dr. Cui identifies.
How do neutrophils kill cancer cells?Neutrophils produce three cancer-killing substances. First, an enzyme (NADPH oxidase) that converts molecular oxygen into superoxide radicals, a destructive form of oxygen, which is converted into hydrogen peroxide, itself a potent tumor cell destroyer, and subsequently is converted into another antiseptic tumor cell destroyer called hypochlorous acid.
Dr. Cui himself has described in detail three internally-produced molecules provoked by cancer-killing neutrophils that produce totally cancer-resistant mice, what Dr. Cui calls “Spontaneous Regression/Complete Resistant (SR/CR) mice.” Dr. Cui theorized that cancer-killing neutrophils employ either perforin, superoxide or nitric oxide in their cancer-killing effect.
So Dr. Cui bred mice that were deficient in each of these three factors to determine which one or if all killed cancer cells. Perforin-deficient bred mice developed about the same immunity against cancer as tumor-resistant mice, eliminating it as a factor. However, there was a far greater anti-cancer response among perforin-negative mice among females. Then the superoxide-negative bred mice were infused with tumor cells, and again a similar immune response as observed among cancer-resistant mice, except again, there was greater survival among female mice. So Dr. Cui put the nitric oxide-negative mice to the same test, injecting cancer cells directly into their bodies, and they also survived about as well as the totally cancer-resistant mice, except, one again, females were twice as resistant as males.
So what Dr. Cui concluded was that if any single factor (perforin, superoxide or nitric oxide) is eliminated, totally cancer-resistant mice still destroy tumor cells and have greater survival. So these are overlapping protective factors. The immune system has marvelous redundancy. By numbers, nitric oxide was proven to be the most potent of these three factors that enables neutrophils to destroy tumor cells.
It is clear, as cancer researchers in Germany have explained, that “the prevailing contemporary strategies of immunotherapy for cancer have focused on the second line of the immune response, the adaptive immune response,” which is in part comprised of T-cell response.
One of the last barriers that protect against cancer is the activity of the immune system, which involves natural killer T-cells, macrophages and neutrophils. Upon activation neutrophils and macrophages are able to kill tumor cells but they can also release free radicals and induce new blood vessels that feed the growth of tumors.
Neutrophils should not always be viewed as one of the “good guys” in the immune response. Such an army of neutrophils can be mounted against invading germs or tumor cells as to cause massive inflammation.
Some researchers say neutrophils “function overwhelmingly against the cancer patient” by enhancing tumor growth.
Some cancer researchers want to limit recruitment of neutrophils at tumor sites in order to inhibit the development of new blood vessels that feed tumor growth.However, efforts have been made to dull the neutrophil response to tumor cells, for instance, by inhibiting interleukin-8, which has been shown to reduce the size and number of tumors. Human clinical studies indicate the presence of neutrophils results in a poor prognosis for the cancer patient.
The idea of employing neutrophils to kill cancer cells has only recently been contemplated. Researchers now understand that neutrophils can polarize the biological action to either neutrophil-type 1 or neutrophil-type 2 which inhibit or promote cancer development.
Aging impairs the activity and numbers of neutrophils, and cancer is largely a disease of aging, so the rationale to employ neutrophils against cancer is logical.
Strikingly, cancer chemotherapy, the mainstay of cancer treatment, induces a shortage of neutrophils (neutropenia), making cancer patients susceptible to treatment-induced infections. Chemotherapy impairs the very cancel-killing effect of neutrophils. .
University of Pittsburgh researchers now propose neutrophils can be controlled in such a manner to kill cancer cells. Heretofore neutrophils were thought only to provoke the massive inflammation that becomes the environment for gene mutations and precancerous states and eventual tumor masses.
Researchers Alyssa D. Gregory and A. McGarry Houghton say it this way:
Although commonly encountered within the tumor microenvironment, neutrophils have not been traditionally considered anything more than a casual observer, and certainly not a disease modifying entity. This view likely reflects disbelief that such a short-lived cell could impact a chronic, progressive disease. However, upregulation of neutrophil–chemotactic substances ensures the constant replenishment of tumor-associated neutrophils (TAN), which are fully capable of modifying tumor growth and invasiveness.Chemotaxis is a phenomenon where the movement of cells like neutrophils are directed towards certain chemicals in their environment, that is, targeted to approach cancer cells and literally blow them up.
However, this does not limit neutrophils to a cancer-killing effect only when their activity and numbers are tamed. Researchers also now realize that neutrophils have a “very powerful anti-tumor effect under certain circumstances.” Acute inflammation can trigger neutrophils to fight tumor cells very efficiently. This runs contrary to what has been presented so far. There are reports of human cancer remissions when a neutrophil stimulator (granulocyte colony-stimulating factor) is used, which stimulates intense and sustained action by neutrophils.
Only very recently have researchers begun to describe the conversion of neutrophils into monster tumor fighters as “an easy way to fight solid tumors.” Researchers say human clinical trials are urgently needed to prove whether neutrophil therapy will provide a new avenue for the clinical treatment of cancer.
Generally, neutrophils have been mischaracterized as tissue-destructive in acute infections. However, neutrophils also release self-controlling factors that limit inflammation and also send signals to activate T-cells. These properties of neutrophils have only recently been appreciated.
The most striking property of neutrophils is their ability to navigate alongside tumor cells and literally blow them up with a burst of oxygen free radicals and reactive nitrogen.
It has been said that neutrophils are “probably the most underappreciated immune cells among the family of white blood cells.”
So what can keep neutrophils under control so they don’t over-respond and create inflammation and tissue destruction? One such neutrophil controller is resveratrol (rez-vair-ah-trol), known as a red wine molecule. When resveratrol was given to mice after they were intentionally fed an iron-rich chemical (dextran sulfate) that induces inflammation in the colon of laboratory mice, inflammation was quelled and the percentage of neutrophils arriving at the scene were reduced. In lab mice it was shown that resveratrol reduces tumor incidence in the colon from 80% to 20%. Resveratrol-treated animals developed only 0.2 tumors per animal compared to 2.4 tumors in untreated animals.
Vitamin B6 appears to play a key role in maintaining adequate numbers of neutrophils. When animals are given a vitamin B6-deficient diet, within two weeks there is a measured decrease in the number of neutrophils. Another finding was that B6 deficiency resulted in shrinkage of the thymus gland, the gland that produces T-cells.
One of the actions of vitamin B6 is to control protein degradation rates. It has been shown that supplemental vitamin B6 reduces degradation of neutrophil proteins. So B6 sufficiency will prolong the life of neutrophils in the blood circulation.
In fact, in a patient with an abnormally low number of neutrophils (a condition called neutropenia), the provision of high-dose vitamin B6 corrected the condition. A shortage of neutrophils appears to encourage the growth of squamous cell skin cancers.
Beta glucans, which enhance the ability of neutrophils and other white blood cells to fight cancer and infections, can also be employed. Beta glucans are sugar-like molecules that are round in bran of cereal grains and the cell wall of Baker’s yeast and many kinds of mushrooms.
Because vitamin D is key in the activation of neutrophils and is a central player in the maintenance of human immunity against cancer, it will be covered in greater detail in this report.
This report began with the presentation of a year-long proven cure for leukemia employing genetically re-engineered T-cells. While vitamin D was discovered decades ago, it is only now being considered for treatment of leukemia.
The use of vitamin D in the treatment of chronic lymphocytic leukemia is not far-fetched. It may have taken a long time in coming, but some researchers now say vitamin D “could potentially modify the natural progression of this incurable disease.”
People residing in the highest northern latitude countries have minimal exposure to the fast-tanning solar ultraviolet-B rays, lower blood serum levels of vitamin D and the highest rates of leukemia.
What is strange is the missing abundance of science regarding neutrophils and vitamin D deficiency. Vitamin D turns otherwise sluggish neutrophils into highly mobile white blood cells that are able to chase down and pursue pathogenic germs and tumor cells.
The importance of vitamin D in neutrophil cancer therapy cannot be overemphasized. Vitamin D is a key factor linking both the early (innate) and delayed (adaptive) immune response. Neutrophils, the first and most abundant responders to invading germs and cancer cells, as part of the innate immune system, also help activate and control the adaptive immune response (T-cells) as well. Vitamin D is at the center of these biological responses to invading pathogens.
The immune system itself contains all the machinery needed to convert vitamin D from its inactive (25-hydroxyvitamin D) to its active form (1,25-dihydroxyvitamin D). Vitamin D controls both neutrophil and T-cell responses. White blood cells called monocytes induce the vitamin D-activating enzyme CYP27B1 which then activates the innate immune response and obviously neutrophils.
Most important, vitamin D inhibits inflammation by suppressing over-active T-cell responses as well as countering overproduction if inflammatory agents nterleukin-2, interferon gamma and tumor necrosis factor (TNF). Interleukin-2 is normally produced by the body during an immune response and is instrumental in the body’s natural response to microbial infection and in discriminating between foreign (non-self) and self.
For example, vitamin D helps to prevent organ transplant rejection yet it does not seem to interfere significantly with protective immune responses against pathogens like bacteria and viruses.
T-cells also have a molecular doorway or receptor for vitamin D. The vitamin D receptor is required for the development of natural killer T-cells, which inhibit autoimmunity (body against itself, or the over-production and activation of immune cells). Vitamin D normalizes the immune response, critically important for making neutrophils the cancer cell killers they are intended to be.
Martin Hewison, a tenacious vitamin D researcher at the David Geffen School of Medicine at UCLA, leads us out of the woods in understanding how this vitamin works in the immune system. Hewison explains that interaction between vitamin D and the human immune system was only documented 30 years ago. However, it has been known for decades that children with rickets (bone softening due to vitamin D deficiency) exhibited chronic infections.
Hewison goes on to document the more recent discovery of vitamin D-activated antibiotic peptides (linked amino acids) called cathelicidins which kill off germs and malignant cells. Prior to this discovery, the key action of vitamin D was believed to be limited to macrophages, a type of white blood cell derived from monocytes that literally ingest roaming microbes and tumor cells.
Hewison also documents that the type of genetically engineered T-cells employed in the recent successful treatment are CD8 T-cells whose surfaces are very sensitive to vitamin D. Vitamin D can regulate CD8-type T-cells following an immune challenge by a pathogenic bacteria, virus or malignant cell.
Hewison makes an important point. A shortage of vitamin D has largely been determined by the presence of bone softening (rickets) in children or what is called osteomalacia in adults. The observation that blood serum concentrations of calcitriol, the active form of vitamin D in the blood circulation, as high as 75 nanomole, normalizes an otherwise overactive parathyroid gland. A human is at risk for bone softening when blood concentration of vitamin D is less than 20 nanomole. That is to say, it takes a much higher blood serum level of vitamin D to prevent excessive parathyroid hormone than it does to prevent rickets.
Given this new definition of vitamin D insufficiency (up to 75 nanomole) to quell an over-active parathyroid gland, it appears a larger percentage of the world’s population is actually vitamin D insufficient than previously estimated.
A search to find whether there is a link between hyperparathyroidism and cancer yields just one limited published report.
Strikingly, it may take as much as 15,000 international units (IU) of oral vitamin D to normalize parathyroid function in some patients with osteoporosis (bone thinning in the latter years of life).
Another intriguing connection between vitamin D and the immunity it confers is its partnership with natural plant molecules called isoflavones or phytoestrogens, such as quercetin, resveratrol and genistein found in concentrated doses in red wine and fermented soy.
Plant estrogens like resveratrol and quercetin may also exert another positive effect in combination with vitamin D. Phytoestrogens also activate toll-like receptors which in turn activate macrophages, an engulfing type of white blood cell, which then increases the sensitivity of the vitamin D cell receptor.
This report started off with the announcement of what appears to be a real cure for leukemia, cancer of the blood. It is not surprising, after what has been learned in this report, that vitamin D is a powerful anti-leukemia weapon. Using a polyphenolic phytoestrogen (carnosic acid from rosemary) to prime vitamin D’s effect, it has been shown in lab dishes that vitamin D plus a phytoestrogen normalizes red blood cells.
For vitamin D to work it must exert its influence via a molecular doorway called a cell receptor site that is tuned to receive specific chemical signals. These receptor sites reside on the surface of living cells including cancer cells. Isoflavones and phytoestrogens sensitize the vitamin D cell receptor located in the surface of living cells, which in turn raises the serum level of the active form of vitamin D via inhbition of a vitamin D-degrading enzyme (CYP24) and by promoting another enzyme (CYP27B1) involved in the synthesis of the active form of vitamin D (1,25-dihydroxyvitamin D(3).
This may also explain why Dr. Zheng Cui’s female lab rats exhibited greater survival than males. Their natural estrogen likely works like plant estrogens to increase the active form of vitamin D as well as its concentration in the blood circulation.
While one study showed only about 30% of patients with chronic lymphocytic leukemia were vitamin D deficient, a non-functioning vitamin D receptor also predisposes to the development of leukemia. High vitamin D cell receptor site expression is, for example, associated with reduced risk for lethal prostate cancer.
Iron is a growth factor for all tumor cells, particularly red blood cells, such as in cases of leukemia where the red hemoglobin pigment transports oxygen and iron. Iron removal (chelating – pronounced key-lay-ting) therapy induces leukemia cells to differentiate into white blood cells (monocytes) rather than red blood cells. About 30% of the genes that are switched on by iron removal are also targeted by vitamin D. Iron chelating agents (like quercetin, rice bran IP6) induce the vitamin D receptor in a synergistic way with vitamin D itself. When leukemia patients do not respond to chemotherapy, iron chelators plus vitamin D act synergistically results in reversal of anemia caused by loss of both red and white blood cells due to the disease.
It will take years for researchers to unravel all the biological vagaries of neutrophils and immunotherapy. It took decades for the T-cell/leukemia cure to become reality for the first three patients. Here cancer patients, and those who are healthy, have an opportunity to get ahead of slowing-moving science.
Cancer patients reading this article don’t have time to wait. They must make decisions about treatment using the best available evidence today. The same it true for patients who have undergone cancer treatment and fear its reoccurrence.
Neutrophils may be THE cure for cancer, and these super-cancer killing cells appear to be weaponized by readily available non-prescription nutrients such as vitamin D3, resveratrol, vitamin B6 and other ancillary factors such as natural iron chelators (IP6 rice bran, quercetin) and immune boosting beta glucans.
While dosing studies are not in hand, modest doses of these nutrients do not appear to be potentially harmful. For those who fear cancer, and they are many, why not heighten your immunity against this long-dreaded disease by taking these dietary supplements beginning today? Since these nutrients are commonly available without a prescription and reasonably affordable, self care is a consideration.
Don’t forget that modern medicine has sophisticated treatments but no cures for cancer. Your insurance plan may pay for whatever your doctor prescribes, but that doesn’t mean it cures.
Many will rush to their doctor with the pages of this report in hand, to inquire of his/her opinion of what has been said here. Anticipate the confounding response that what is proposed in this report “is yet unproven.” Yes, but what oncologists prescribe for cancer today is already disproven. It is illogical to compare something new against something that has been shown not to work.
Cancer patients often make treatment decisions out of fear and ignorance, and having little understanding of their own disease and little time to assess any alternatives, are forced to rely upon their doctors to make decisions for them.
Frankly, this writer’s experience is that few cancer patients will have the gumption to put any of what has been written here into practice. At best, cancer patients will elect to undergo chemotherapy, radiation treatment or surgical excision of their tumors, which often leads to patients succumbing to treatment before they succumb to their disease.
Most cancer patients will elect to obtain the best of both worlds and undergo conventional toxic cancer therapy AND alternative therapies. Many won’t seek alternatives till all conventional treatments have been exhausted and their finances and willingness to fight cancer have been depleted. They won’t realize the futility of modern cancer care till it is too late.
Here and there modern medicine concedes its toxic cancer treatment are ineffective and at best prolong life just a few months, and at great expense and with considerable side effects.
The best cancer care would require no doctoring at all. After spending billions on cancer research, it is odd that the field of oncology hasn’t one proven approach to cancer prevention beyond smoking cessation. Even the federal government program that encouraged Americans to consume 5-servings of fruits and vegetables daily did not reduce mortality rates for cancer or heart disease for that matter. The army of cancer doctors, hospitals and clinics are adept at detecting cancer and collecting insurance payments. Prevention is an unmentioned topic among oncologists. The ethical goal of oncologists would be to put themselves out of business. Instead, we see the opposite. Over-diagnosis and overtreatment abounds. Cancer is a jobs program and cancer had better not disappear any time soon.
Will you or your family have the nerve and common sense to put what has been said here into practice? Oftentimes cancer patients are so ill their loved ones make decisions for them. But disagreement among family members is common. Out of fear and the false security that a medical diploma on the wall of a doctor’s office provides the best source of information, cancer patients spend the last days of their lives hoping that what didn’t work for the previous patient will work for them.
Tumor resistance to chemotherapy is inevitable and without exception. A false hope is created for a short time as the tumor shrinks, but then the drug no longer works and chemotherapy destroyed the patient’s last hope — their immune system.
The main objective in cancer prevention should be to maintain summer-season cancer resistance by supplementing the diet with vitamin D pills plus important co-factors like resveratrol and vitamin B6 that weaponize neutrophils to kill roaming cancer cells. — © 2011 Bill Sardi, Knowledge of Health, Inc. Not for posting on other websites.
Posted in Cancer ; No Comments »
You must be logged in to post a comment.
11
17
52
95
14
24
237
6
56
43
10
116
15
66
105