Posted October 25, 2017: by Bill Sardi
Low thyroid hormone levels can result in mental confusion. Which only adds to the bewildering state of affairs when it comes to recognizing and rectifying low or high thyroid hormone levels.
While thyroid hormone dysfunction affects 1% of the general population it affects 10% of senior adults (10% females; 6% males).
Many millions of Americans rely on thyroid hormone replacement. But about as many (13 million estimated) may have low thyroid levels and don’t know it.
To make matters worse, an estimated 40% are over-treated; 48% undertreated. Wary of overtreatment which can lead to bone loss and irregular heart beats, many physicians are hesitant to prescribe thyroid hormone replacement, particularly in the oldest old.
The biggest problem is that in 90% of subjects with low thyroid (hypothyroid) their thyroid gland is under attack by their immune system. This autoimmune form of thyroiditis is poorly addressed by modern medicine, which is a focus of this report.
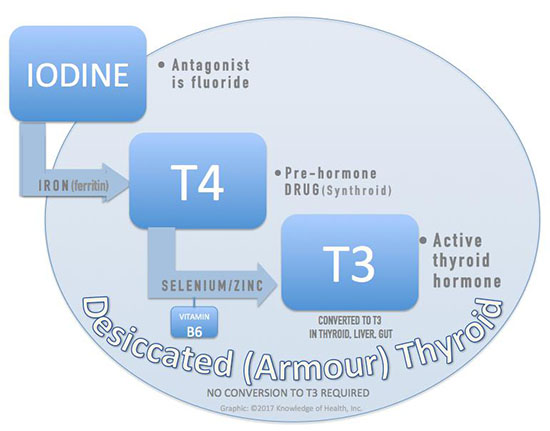
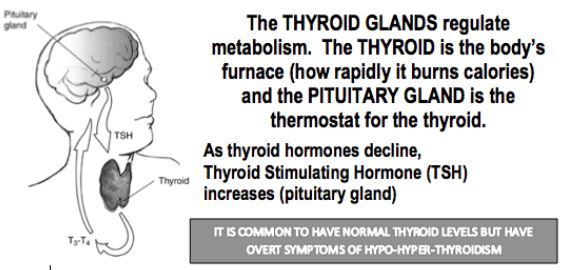
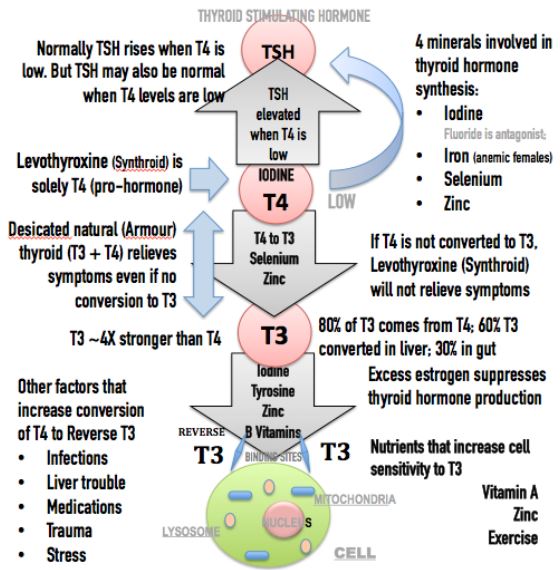
Before you go on reading this report, an oversimplified primer on how the thyroid gland works is in order. The thyroid gland regulates your metabolism, that is, the rate at which your body burns calories. High thyroid hormone and you feel hot, your heart rate increases and you lose weight. Low thyroid and your heart rate slows, even your speech slows, you gain weight and feel cold. The thyroid gland makes T4 hormone (iodine). If insufficient T4 then Thyroid Stimulating Hormone (TSH) is produced in the pituitary gland located at the base of the brain. A high TSH level is the lazy doctor’s way of diagnosing low (hypo) thyroid. T4 must convert to T3, the active hormone. The leading brand of synthetic thyroid replacement is solely T4. There is also natural desiccated thyroid from animal source that provides T4 and T3 that modern medicine largely snubs. High (hyper) thyroid that often occurs from overdosing thyroid hormone. The biggest problem with thyroid hormone replacement is lack of absorption. Now you are ready to learn why all this goes haywire.
There are at least 25 ways thyroid hormone replacement can baffle even the most expert of endocrinologists.
Low iron levels, particularly in young females, may induce hypothyroidism. This is usually due to heavy prolonged menstrual flow. But also because high estrogen levels interfere with thyroid metabolism by increasing proteins that bind to thyroid hormone. A GI tract enzyme called beta glucuronidase reactivates estrogen. Cruciferous vegetables (broccoli, cauliflower, cabbage, Brussel’s sprouts, kale) help lower beta glucuronidase by their calcium glucarate content. Calcium glucarate is also available as a dietary supplement.
If relying upon blood tests to determine anemia, obtain a ferritin test. It is iron storage protein (ferritin) levels that correlate with a higher T3 to T4 ratio. Normal range of ferritin is 20-70.
The human body normally secretes T4 over T3 in an 11:1 ratio. However, levothyroxine (Synthroid), the most widely prescribed thyroid pill, only provides T4. While some alternative medicine physicians resorted to using T3-T4 combination desiccated (Armour) thyroid when Synthroid (T4) failed to produce resolution of symptoms, this occurred in an era when physicians failed to recognize thyroid T4 is poorly absorbed for a variety of reasons described elsewhere in this report. Thyroid tablets were also found to be unstable and have a short shelf life and were being stored improperly by many patients, further robbing hypothyroid patients of a symptomatic cure.
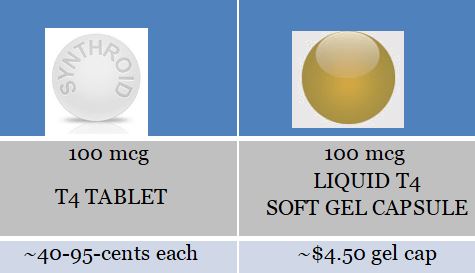
Poor absorption of T4 pills (Synthroid and other brands) often led physicians to needlessly increase dosage. The poor absorption of levothyroxine (T4-Synthroid) finally led to the recent availability of liquid T4 in soft-gel capsules that largely resolves the problem of malabsorption and eliminates the need for patients to take their thyroid pills 60 minutes prior to meals, which led to very poor patient compliance. Soft-gel T4 capsules have been demonstrated to overcome the well-known problem that coffee poses to T4 absorption. Hypothyroid patients no longer need to avoid coffee or take their pills an hour prior to eating, which should improve compliance.
And it is noteworthy to mention liquid T4 in soft-gel capsules even improves absorption among patients with no malabsorption disorders.
The problem with soft-gel liquid T4 capsules is that the manufacturer is guilty of price gouging. A 100-microgram T4 Synthroid tablet ranges from ~40-94-cents each. Whereas the liquid T4 sells ~$4.50 per soft-gel cap. Otherwise thyroid sufferers could all switch to the soft-gel capsules and be done with many of the problems associated with hypothyroid therapy. One wonders if the pharmaceutical companies are making thyroid tablets that don’t properly dissolve on purpose so as to force the liquid soft-gel capsules to be prescribed.
Now for a zinger. A shocking reality is that 90% of cases of hypothyroidism are among people (largely women) who have Hashimoto’s thyroiditis. This is an autoimmune disorder. This means the immune system is attacking the thyroid gland, thus impairing production of T4 and T3.
This is not just an age-related withering of the thyroid gland. It is destruction of the glandular functions of the thyroid. Blockage of antibodies that attack the thyroid gland may switch from a hypothyroid to a hyperthyroid state. Many other autoimmune disorders (psoriasis, rheumatoid arthritis, type I diabetes, multiple sclerosis, lupus, alopecia, Graves disease, inflammatory bowel disease, to name a few) are associated with hypothyroidism.
Typically when autoimmune thyroiditis gets out of control, either prednisone (steroid) or immune suppressant drugs are prescribed. But these are fraught with side effects. Some doctors even resort to surgical removal of part of the thyroid gland. This is an overkill.
Very intensive statin drug therapy may reduce thyroid autoimmunity but very high doses which could be liver toxic (20-40 mg) are required. And the combination of statin drug therapy and hypothyroidism appears to increase the risk for muscle pain (rhabdomyolysis).
Modern medicine is side-stepping whatever is causing a massive epidemic of autoimmune disorders and just treating symptoms. Steroidal medication (prednisone) is employed simply as an anti-inflammatory agent, but is not curative for hypothyroid.
In the case of hypothyroidism, the autoimmune reaction is allowed to go unabated, mostly because of the side effects of drugs used to quell autoimmunity.
As a report published at Atlas of Science points out, the lack of zinc (or balance of zinc with copper) is at the heart of autoimmune disorders.
The lack of zinc not only impairs the thyroid gland, it causes the thymus gland that makes T-cells to shrink also.
Selenium, another prominent trace mineral that is involved in the conversion of T4 to the active T3 form of thyroid hormone is critical in the activation of enzymes (deiodinases) that regulate T3 levels. Selenium supplementation seems to favorably alter the immune response in autoimmune thyroiditis.
The highest selenium content is found in the thyroid gland. Selenium activates an antioxidant enzyme (glutathione peroxidase) that protects the thyroid form excess hydrogen peroxide.
Selenium is considered adequate in the American diet. However, experts point to impaired gastrointestinal absorption of selenium. A few years back it was reported that selenium could play a therapeutic role in thyroid inflammation.
Among women with high estrogen levels in the postpartum period, selenium was found to dramatically reduce hypothyroidism (from 48.6% to 28.65%). Pregnancy obviously raises estrogen levels that increase the need for selenium in the control of thyroid hormones.
While zinc supplementation doesn’t always improve thyroid dysfunction, this could be explained by poor absorption of zinc that is vastly improved by combination with vitamin B6, and poor bioavailability of zinc as it is bound tightly to a transport protein (metallothionein). Selenium facilitates the release of zinc from its binding protein. Vitamins A & D improve zinc absorption. So does vitamin B6.
Another recent study found the ratio of copper over selenium to be a significant factor among patients with Hashimoto’s thyroiditis.
This is just maddening. How does anybody find their way out of the thyroid maze? It appears a thyroid hormone imbalance requires an encyclopedia of knowledge that challenges even the best endocrinologist.
Given that most cases of hypothyroid involve autoimmunity, and modern medicine has nothing but problematic immune suppressant drugs, hypothyroid patients should attempt to quell the fires of autoimmunity with zinc and selenium along with vitamin B6 to enhance zinc absorption.
What is needed is a miracle molecule to quell the ravages of hypothyroidism. Resveratrol, shunned and dismissed by modern medicine is that molecule.
While the masses wait for a sign from heaven to cure their insidious thyroid hormone imbalance, they should consider resveratrol pills as it is becoming increasingly clear resveratrol is the human body’s middle-age reset switch.
Just when the thyroid gland, the body’s thermostat for calorie burning, begins to malfunction— resveratrol comes to the rescue.
Only recently has it become clear that resveratrol helps to overcome low-thyroid conditions that are closely associated with mental depression and memory problems.
In recent years evidence has accumulated to show resveratrol enhances thyroid function.
Finally, resveratrol may tackle a medically challenging metabolic problem – that of subclinical low thyroid (hypothyroidism). Subjects with this condition don’t exhibit full-blown thyroid collapse with accompany weight gain and coldness but do experience anxiety and mental depression. Mental decline and learning problems are other manifestations of this thyroid disorder. Approximately 4-20% of adult populations have this hypothyroid condition, which is treated by prescription for T4 (thyroid 4) hormone.
However, proper dosing of T4 is difficult to determine and patients may experience side effects from overdosing such as racing heart, angina (chest pain) and nervousness. The need for better medicines to treat subclinical hypothyroid is large.
Subclinical hypothyroid is confirmed by elevated levels of thyrotropic-stimulating hormone (TSH) with other thyroid hormones in the normal range.
Here is what happened when laboratory mice were given T4 or resveratrol for their chemically induced hypothyroid condition (see chart below). Note the remarkable almost 4 fold reduction in TSH levels (2.49 to 0.65) in resveratrol-treated mice!
In the laboratory, resveratrol alleviated anxiety and depression in animals with subclinical hypothyroidism. Laboratory mice had their thyroid glands cauterized so only half of the lobes were operative in order to impair learning and memory. Then resveratrol was given with levothyroxine T4 and TSH levels dropped and the learning and memory problems were remarkably reversed! Resveratrol could become every thyroid hormone users best friend.
Note: This condition is confirmed by elevated thyrotropic stimulating hormone (TSH) levels. Resveratrol compares favorably with T4 therapy without inducing potential side effects.
|
T3 |
T4 |
TSH |
|||||
|
Before |
After |
Before |
After |
Before |
After |
||
|
Resveratrol |
0.73 |
0.56 |
8.88 |
6.71 |
2.49 |
0.65 |
|
|
T4 |
0.74 |
0.91 |
835 |
13.97 |
1.43 |
0.14 |
|
| Sources: Frontiers Endocrinology 2016; Endocrinology Journal 2015 | |||||||
Whether endocrinologists are ready to prescribe resveratrol for this common condition is unknown.
More remarkably, in a 26-week study involving laboratory mice, two polyphenols, resveratrol and quercetin along with lipoic acid, an antioxidant naturally produced in the body and available as a dietary supplement, overcame high-fat diet- induced thyroid hormone abnormalities that usually lead to weight gain, elevated blood pressure and reduced antioxidant defense.
Resveratrol by virtue of its ability to enhance iodine (iodide) maintained high metabolism and averted weight gain typical experienced among animals whose thyroid hormones are disturbed by a high-fat diet. While mice on a high-fat diet developed resistance to a satiety hormone (leptin) and therefore eat more food, resveratrol, quercetin and lipoic acid inhibited this.
|
Regular Diet |
High-fat diet |
High-fat diet + resveratrol |
High-fat diet + quercetin |
|
|
TSH |
526.1 |
604.6 |
677.5 |
633.6 |
|
T4 |
181.6 |
208.5 |
198.0 |
186.3 |
|
T3 |
20.5 |
13.7 |
18.6 |
17.1 |
|
Antioxidant capacity |
0.401 |
0.487 |
0.555 |
1.057 |
|
Glutathione |
0.598 |
0.482 |
0.553 |
0.524 |
|
Catalase |
36.02 |
15.96 |
40.18 |
44.95 |
Source: Journal Nutritional Biochemistry 2016
Resveratrol has even been shown to counter the antagonism of iodine by fluoride, which naturally occurs in groundwater or is added to harden tooth enamel and reduce dental decay.
In another experiment, among laboratory mice whose ovaries had been removed to replicate menopause, low-dose resveratrol increased T3 hormone levels.
©2017 Bill Sardi, Knowledge of Health Inc.
| Underactive Thyroid Hypothyroid |
Normal Thyroid Euthyroid |
Overactive Thyroid Hyperthyroid |
|---|---|---|
| 9% of Adults | 1% of Adults | |
|
13 milion Americans have undetected underactive or overactive thyroid glands; 1% of adults overall; 10% of elderly; by gender: 10% of females, 6% of males |
||
| 90% hypothyroid have autoimmune thyroiditis (Hashimoto’s) | Goiter: enlarged thyroid gland (swelling base of neck); Grave’s disease | |
| Body is cold; axillary (underarm) temperature upon awakening in AM is under 97.4° Fahrenheit | Normal axillary temperature; 98° Fahrenheit in AM upon awakening. Oral temperature 98.6° – 99.0° Fahrenheit (37.0°-37.2° Celsius) | Subject feels hot; axillary (underarm) temperature is above 98.6° Fahrenheit |
| Weight gain | Weight loss | |
| Fatigue, puffy face, joint stiffness, muscle pain, constipation, dry skin, brittle nails, thinning hair, depression, decreased sweating, slow heart rate, hoarseness, slow speech, loss of taste and smell, bloating | Rapid heart beat, fatique, palpitations, inscreased appetite, hand tremor, sweating, more frequent bowel movements, muscle weakness, insomnia, thin skin, brittle hair, bone loss, nervousness, anxiety | |
| Slow pulse under 85 beats per minute | Resting pulse over 85 beats | |
| Condition | TSH | T4 | FT4 (free unbound thyroxine) |
|---|---|---|---|
| Hyperthyroid | Low | High | High |
| Hypothyroid | High* | Low | Low |
| Hypothyroid (pituitary) | Low | Low | Low |
*Not always
Graphics: © Knowledge Of Health, INC
Posted in Dietary Supplements ; No Comments »
11
17
52
95
14
24
237
6
56
43
10
116
15
66
105