Posted November 29, 2017: by Bill Sardi
The following report links high blood pressure (hypertension) to a shortage of zinc due to poor dietary intake, impaired absorption and/or lack of bioavailability. The report is requisitely lengthy to fully document the problem to the scientific community and other demanding reviewers. For time-pressed readers, the first four pages cover the main findings of this report.
The issue of whether zinc is involved in the etiology of hypertension has been mired in confusion for years as various animal and human studies employed overdoses of zinc, which actually does induce hypertension.
However, a compelling quadratic intersection of geographical factors, reported for the first time in this report, provides compelling evidence that hypertension emanates from poor zinc nutriture.
Southern States are (1) where the so-called “stroke belt” of the United States is located; (2) have the highest intake of salt; (3) have the lowest soil levels of zinc and (4) the highest blood pressure numbers.
Poor zinc nutriture leads to taste insensitivity and an increase in salt consumption, which leads to hypertension. The surprising remedy to salt craving is zinc, not abstention from salty foods as often recommended by health authorities.
What readers want to know, before they have to labor through this entire report, is how to resolve this problem. The best answer is to turn to dietary supplements, as it is difficult to assuredly resolve shortages of zinc from the diet.
The best diet consisting of 5-9 servings of fruits and vegetables will not provide sufficient amounts of zinc. An adult would have to consume a cup of wheat germ, or ten cups of cooked spinach, or 2 cups of pumpkin seeds or nuts to obtain 15 milligrams of zinc per day (the Recommended Daily Allowance). Nor will omnivorous or carnivorous (meat eating) diets likely provide sufficient amounts of zinc either. Two pork or chicken steaks a day would provide ~15 mg of zinc.
In addition to finding the best source of zinc (widely sold zinc oxide is the most economical but also insoluble in water), nutritional co-factors are needed to facilitate proper absorption (vitamin B6) and release (selenium) of zinc. Furthermore, folic acid, vitamin E, potassium and especially magnesium have been revealed in this report as blood pressure controllers. For these nutrients, a multivitamin would be the most practical and economical way to achieve zinc adequacy.
To that end, the MOLECULAR MULTI has been formulated. It is the only multivitamin that adequately corrects a widespread zinc deficiency in the population (30 mg of zinc citrate) with needed co-factors (vitamin B6, selenium).
The provision of other minerals, namely magnesium, in supplement form, can also help negate the hypertensive effect caused by a shortage of zinc. Since magnesium is a bulky mineral, it must be obtained as a separate dietary supplement.
This report has been written in the wake of a newly issued report from the American Heart Association that calls for adults to be treated for hypertension when their blood pressure rises to 130/80 instead of the old standard of 140/90.
Before millions more American adults are placed on ineffective and problematic blood pressure pills, they should be informed three of the major classes of blood pressure drugs (diuretics, ACE inhibitors and vasodilators) deplete the human body of zinc and forever ensure patients will remain hypertensive and totally reliant upon drugs to control their blood pressure. Safe weaning away from blood pressure drugs would require zinc supplementation.
Blood pressure pills are a bonanza for Big Pharma as no single anti-hypertensive drug is effective. Most patients are placed on two or three drugs to bring their blood pressure under control. Drug-induced side effects are common, with chronic cough emanating from the use of ACE inhibitors affecting 10% of users.
It cannot be construed or advertised that any zinc supplement prevents, treats or cures any disease says the Food & Drug Administration, until proven in a conclusive human study. However, that would categorically make zinc a high-priced drug. It would be absurd to think a zinc tablet would be classified as a drug.
While matching the latest science, the MOLECULAR MULTI remains untested for this purpose and would be classified as a drug if it did was in fact proven lower blood pressure. So no health claim can be made for this or any other disease.
The FDA’s rules are preposterous, preventing a free market for natural versus synthetically made medicines, particularly when the origin of hypertension is a trace mineral deficiency that could be quelled by a zinc pill.
A human clinical study involving a dietary supplement to prove the point made in this report is way overdue and is not likely to be forthcoming. The National Institutes of Health aids and abets the problem by nor sponsoring definitive studies. It seems unconscionable to allow the American public to be conned by drug companies who in a covert manner, employ zinc-depleting drugs that makes patients totally dependent on their drugs for the remainder of their lives.
At the very least, if hypertension is a health issue for you, find a zinc pill and avoid zinc oxide that is the most economical form but is insoluble in water and should never be sold. Add a magnesium tablet for best effect.
For answers to further questions about this topic you may reach me at here
Bill Sardi
The definition of high blood pressure may have just taken a plunge with the American Heart Association issuance of new guidelines that recommend treatment for hypertension should begin at 130/80 rather than 140/90.
Regardless of treatment blood pressure still remains out of control for many Americans whether on drug therapy or not. A concealed cause of hypertension is a shortage of an essential mineral, kept hidden from view while more and more mineral-depleting drugs are employed to ensure hypertension is never cured.
Zinc is the unexpected mineral that controls blood pressure as described in the medical literature but not heeded by practicing physicians.
To confirm the zinc origin of hypertension, four compelling geographical factors intersect and are involved in the occurrence of stroke and hypertension in the U.S.: (1) the so-called “stroke belt in the U.S. is in Southern States; (2) Southern States have the highest sodium consumption in the U.S.; (3) Zinc soil levels are lowest in the Southern States; (4) Blood pressure is highest in Southern States.
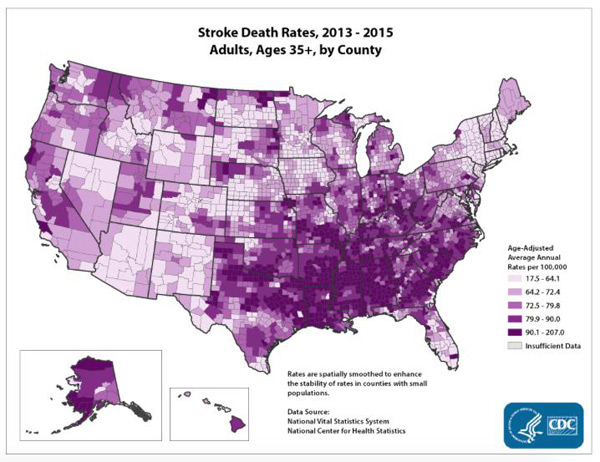
A problem is that this knowledge is not incorporated into any public health practices. Efforts to truly prevent salt-induce hypertension via adherence to sodium-restricted diets have been disappointing. It appears food fortification with zinc could erase much of the risk of hypertension. This idea is not on the drawing board by public health authorities. For now, hypertension will remain a malady that is treated, for all practical purposes, as a drug deficiency.
There are two ways a shortage of zinc produces hypertension.
To elucidate further on this second underlying mechanism that breeds hypertension, zinc is required for the production of nitric oxide synthase, an enzyme that produces nitric oxide gas within arteries. Nitric oxide (NO) dilates or widens blood vessels, thus controlling blood flow and pressure. A shortage of zinc induces the superoxide radical (unbalanced electrons in atoms) that creates tissue-destructive oxidation. It is the superoxide radical that negates nitric oxide. Zinc is required to produce superoxide dismutase (SOD), the enzyme that counters the superoxide radical.
A chart is provided below to help understand the complex factors surrounding zinc deficiency that results in hypertension.
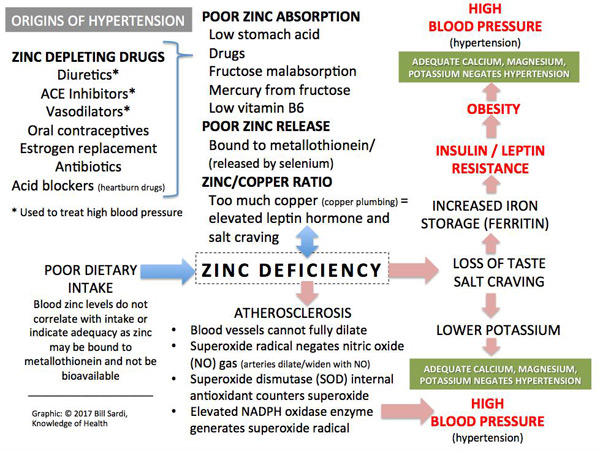
According to published studies, it appears that sufficient calcium, potassium and especially magnesium serve as a backstop to help negate the hypertensive effect of zinc deficiency and promote normal blood pressure.
Advancing age and obesity are said to be the two strongest risk factors for uncontrolled blood pressure. But zinc is overlooked. Zinc blood levels decline with advancing age.
A landmark report notes that a deficiency of zinc may ignite overeating by impairing taste acuity, which results in overuse of salt that in turn increases blood volume and elevates blood pressure.
Zinc and copper must be balanced. A copper deficiency results in weak connective tissue and unstable heart and arteries. The relationship between zinc and copper may be a predominant balancing act to maintain health in a developed country that consumes mineral-less processed foods. The ratio of zinc over copper is diminished among hypertensive individuals. In response, public health authorities do nothing outside of over-drugging the population.
In a zinc deficient population, excessive salt-induces fluid overload that leads to release of renin from the kidneys, a hormone that increases blood pressure. Renin generates angiotensin converting enzyme (ACE) that converts to angiotensin II, a hormone that constricts arteries and raises blood pressure.
ACE inhibiting drugs predominate in modern medicine’s effort to control blood pressure. But ACE inhibitors deplete zinc. It becomes apparent that the failure to correct the zinc/copper imbalance results in marginal effects by synthetic drugs to overcome this dire situation, which is a likely reason why multiple drugs are required to bring blood pressure under control.
Copper, commonly obtained from copper plumbing and copper in dietary supplements, is associated with an unbalanced zinc/copper ratio, which in turn increases leptin, an appetite controlling hormone secreted by fat cells. Overproduction of leptin or leptin resistance can also induce salt retention and result in hypertension.
Thiazide diuretics, considered the first line of treatment for hypertension, are also reported to induce zinc deficiency.
And it’s not just the anti-hypertensive drugs that induce zinc deficiency. Drugs prescribed for heart failure have the same drawback.
Of additional interest, magnesium deficiency is reported to induce resistance to antihypertensive drugs.
Aside from copper plumbing and copper in dietary supplements, there are other ways the zinc/copper balance is altered. When fruit sugar (fructose) was added to the diet of laboratory animals (hamsters) and half of the sugar-fed animals were given supplemental zinc, the arteries of zinc-fed animals were less dysfunctional in regard to arterial dilatation.
Another interesting cause of zinc deficiency is fructose malabsorption. Zinc absorption and transport may be impaired when fructose is not absorbed properly. A convincing study showed all of the patients with gastric complaints with low blood serum zinc levels suffered symptoms produced by fructose malabsorption.
Fructose malabsorption is not some rare malady. An estimated 36% of the European population has fructose malabsorption and roughly one half are symptomatic.
When laboratory rats are fed a high fructose sugar diet, a reduction of catalase, an internal enzymatic antioxidant, is noted. Fructose-fed animals experience a rise in blood pressure (128 vs. 109 systolic blood pressure in control animals).
Throw high-fructose corn sugar into the American diet and the problem worsens. Fructose sugar is also known to reduce copper and selenium levels. Increased fructose intake is associated with elevated blood pressure. Increased salt absorption and decreased salt excretion in fructose-fed lab animals strongly suggests fructose contributes to hypertension.
Consumption of high fructose corn syrup is in modest decline in America (now ~41.4 pounds a year, down from 62.5 pounds), but it also portends another ignored origin of hypertension– mercury. Some fructose-sweetened foods and beverages may contain detectable levels of mercury. Mercury consumption can lead to zinc losses.
Mercury is known to impair arterial dilatation, diminish the beneficial effects of omega-3 oils, and increase risk for hypertension. Mercury binds to metallothionein and substitutes for zinc, copper and other trace minerals, rendering these minerals non-bioavailable, which negates the proposed health benefits from these essential minerals.
A prospective study of American men and women showed that mercury levels, even at intakes 2.5 times above the level allowed by the US Environmental Protection Agency, did not increase the risk for hypertension. However, the study population used to come to this conclusion was dominated by younger adult women (nurses) age 30-55 years of age who do not typically exhibit hypertension. According to data provided by the Centers For Disease Control, the risk for hypertension begins to rise after age 55. This kind of study cannot be used to justify avoidable levels of mercury in foodstuffs, as there is no safe level of mercury exposure.
The medical literature explains that the link between zinc deficiency and hypertension is unclear and marked by contrary studies. But those studies often employ overdoses of zinc (example; 100 mg zinc/day) to come to that conclusion.
For example, in one animal study lab rats which range in weight from 300-500 grams were fed 50 milligrams of zinc per 100 grams body weight or ~150-250 milligrams of zinc which resulted in elevated blood pressure. For comparison, a 160-pound human weighs 72,574 grams. The equivalent human dose given to these animals would have been 725 milligrams. That would equal twenty-four 30-milligram zinc pills. Someone would have to intentionally overdose to consume that amount of zinc.
One published review of zinc health requirements suggests the difference between zinc deficiency and zinc overdose (toxicity) is narrow. But the alleged risk of zinc toxicity appears to be theoretical. While dire effects of zinc deficiency are well documented, the practical threat of zinc toxicity from the diet or food supplements appears to be specious.
Ananda S. Prasad, the reigning authority on zinc nutrition, says: “In comparison to other race elements…. Zinc is relatively nontoxic.” The hazard posed by excess copper rather than zinc is what needs to be emphasized.
As evidence, a study of 3718 residents of Chicago over age 65 who took copper supplements (2 milligrams/day) combined with a high saturated fat diet had a 6.51 times greater rate of mental decline compared to persons not taking multivitamins with copper.
In another study published in the Archives of Internal Medicine, copper in multivitamins was shown to produce a mortality rate of 18% among 38,772 women (age 55-69) compared to 3% absolute increased risk of dying from supplemental zinc, which was considered statistically insignificant. That is a six-fold relative increase of premature death.
The most recent human study of zinc and hypertension was published in 2016. That study concluded there was no evidence that higher dietary intake of zinc increases the risk for hypertension but higher blood serum levels of zinc ARE weakly but positively associated with hypertension in males. But the study population was located in Finland where alcohol consumption among males is very high compared to other countries. Alcohol depletes zinc and induces iron overload.
Furthermore, these men were divided by those who consume less than 14.3 milligrams of zinc per day versus those who consumed 14.3 or more milligrams of zinc per day. Among 1652 study participants, dietary zinc intake was evenly divided (826 in the low zinc group and 826 in the high zinc group). In the low zinc group (less than 14.3 mg/day), 13.5% developed hypertension while in the high zinc group (more than 14.3 mg/day) 17.8% developed hypertension (about 32% relative difference, or in absolute numbers a 4.3% difference). Study subjects were asked to abstain from alcohol for 3 days prior to testing.
A 10-to-1 ratio of zinc over copper intake is recommended. Otherwise, adverse effects are of concern. There is little or no evidence that copper deficiency induced via overdose of zinc, in amounts well in excess of the Recommended Daily Allowance (100-300 mg vs. an RDA of 15 mg zinc/day), actually occurs.
The safe upper limit or no observed adverse effects level for zinc ranges from 35-45 mg/day for adults as established by a number of health agencies. One study showed that 45 milligrams of zinc gluconate per day does not decrease copper.
One study indicates less than 0.8 milligrams of copper per day leads to copper attrition while 2.4 milligrams or more lead to copper overload.
The human body stores ~100 mg of copper and 2000-3000 milligrams of zinc.
Oral absorption of copper is reported to be ~50%. Copper absorption can range from 12-71%. Absorption of zinc is 20-30% with a 10-milligram dose.
Zinc supplements vary in the amount of elemental zinc they provide (the remainder is the carrier molecule like gluconate or sulfate). Here is a comparison of some of the forms of zinc used in dietary supplements:
So a 50 mg gluconate zinc tablet would provide ~7 milligrams of elemental zinc and maybe 20-30% of that is absorbed, for a net intake of 1.4 to 2.1 milligrams in the bloodstream. Taking calcium pills, or zinc-blocking medicines, could further reduce the amount of zinc actually getting into the bloodstream. Zinc oxide, the most inexpensive zinc tablet sold, is very insoluble in water and would further reduce the amount of zinc absorbed.
So it would be easy to see why zinc supplementation would never significantly increase blood levels. You take a zinc gluconate supplement labeled for 50 mg of zinc and realize less than 2 mg.
Zinc supplements may supply a much lower level of elemental zinc than the label indicates and then only small amounts of elemental zinc may be absorbed. What results is an imagined zinc adequacy and blood levels that don’t correlate with intake levels from the diet or supplements, which is what is repeatedly reported in the medical literature.
Consumers take zinc supplements to eliminate nutritional gaps in their diet. The US Department of Agriculture says only about 29% of Americans are deficient in zinc. One dated study showed 35-41% of males and 36-45% of females consume inadequate amounts of zinc from their diet and may need to rely on zinc pills, particularly vegetarians and alcohol imbibers.
Modern medicine is lulled into thinking only 35-45% of American adults don’t consume adequate amounts of zinc when the deficiency is likely more widespread and severe.
Modern medicine is making a “killing” off of drugs that deplete zinc and forever induce chronic disease and death. The global anti-hypertensive drug market is expected to reach $24.3 billion by year 2021.
The frequency with which the target blood pressure number is achieved with a single drug is low.
For example, amiodipine (Norvasc), a calcium blocker, and indapimide (Lovol), a diuretic/vasodilator, are drugs used to control blood pressure. Both of these drugs have been found to disturb the zinc/copper ratio. Use of these drugs may require corrective mineral supplementation.
It appears all patients taking high blood pressure pills ought to supplement their diet with zinc. A study conducted in Europe among patients taking all of the classes of drugs (beta blockers, calcium blockers, diuretics, ACE inhibitors) used to treat high blood pressure experienced a decline in their zinc levels. These patients also experienced a rise in blood glucose. When a corrective diet with fortified minerals was consumed with these drugs, zinc levels rose.
Here is an expansive list of most of the zinc depleting drugs that are employed to treat high blood pressure:
ACE Inhibiting medication for high blood pressure: Benazepril (Lotensin), Captopril (Capoten), Enalapril ((Va- sotec), Fosinopril (Monopril), Lisinopril (Prinivil, Zestril), Moexipril (Univasc), Quinapril (Accupril), Ramipril (Al- tace), Trandolapril (Mavik)
Angiotensin II Receptor Antagonist medication for high blood pressure: Candesartan (Atacand), Irbesartan (Avapro), Losartan (Cozaar), Olmesartan (Benicar), Telmisartan (Micardis), Valsartan (Diovan)
NSAID drugs for inflammation: Celecoxib (Celebrex), Diclofenac (Voltaren),Diflunisal (Dolobid), Etodolac (Lodine), Fenoprofen (Nalfon), Ibuprofen (Advil, Motrin, Nuprin), Indomethacin (Indocin), Naproxen (Aleve, Anaprox, Naprosyn), Oxaprozin (Daypro), Piroxicam (Feldene), Sulindac (Clinoril), Tolmetin (Tolectin)
Corticosteroid drugs for inflammation: Beclomethasone(Beclovent,Vancenase,Vanceril), Budesonide(Pul- micort, Rhinocort), Dexamethasone (Decadron), Fluticasone (Flonase, Flovent), Hydrocortisone (Cortef), Mometasone (Nasonex), Prednisone (Deltasone, Meticorten), Triamcinolone (Azmacort, Nasacort)
Tetracycline antibiotics: Doxycycline (Doryx, Periostat, Vibramycin), Minocycline (Minocin), Tetracycline (Achromycin, Sumycin)
Blood serum zinc levels are notoriously misleading. The importance of a program to establish zinc adequacy in a well-fed developed country like the U.S. where zinc shortages (low intake, poor absorption, lack of bioavailability) are rampant, may lead to clinical confusion because even a modest increase (4 mg/day) of dietary zinc improves DNA repair even though there is no increase blood plasma zinc levels.
The US Department of Agriculture reports that ~28% of the American population consumes an inadequate amount of zinc, but that doesn’t consider zinc is poorly absorbed and is often bound so tightly to its binding protein (metallothionein) that it is not bioavailable.
Furthermore, as more zinc is consumed, absorption declines. In one study zinc absorption from the diet ranged from 19-22% but from supplements only 8-10%. This must be a compensating mechanism to prevent zinc overload. So zinc blood levels tend to remain constant regardless of zinc intake.
Doctors who claim dietary supplements are of no value unless a deficiency is indicated by a blood test are ignorant of all this science. One of those anti-dietary supplement doctors has even branded this author as a “public danger” for saying so. This author finds many doctors are commonly camped in their anti-dietary supplement positions, unwilling to recognize the science. Don’t be persuaded by a unreliable blood test that you don’t need to add zinc to your diet.
The kidneys are often involved in the onset of hypertension. Zinc participates in the regulation of blood pressure and kidney function. A reduction in nitric oxide gas to dilate arteries in the kidneys, induced by the superoxide radical, is the underlying mechanism that has been identified. Zinc, via its ability to activate SOD (superoxide dismutase), counters the effect of superoxide that impairs blood flow in the kidneys.
Advanced-stage kidney disease is often accompanied by high blood pressure. But not all kidney disease patients experience hypertension. An animal study reveals that a high-salt diet in salt-sensitive animals produces the superoxide radical that induces the kidney failure. The provision of vitamin E as alpha tocopherols normalizes kidney function among salt-sensitive lab animals.
Not all salt-sensitive lab animals develop hypertension when fed sodium. Only when there are elevated levels of angiotensin-2, a hormone that interferes with nitric oxide gas formation in arteries, do arteries fail to dilate (widen) to control blood pressure.
L-arginine an amino acid known to induce dilatation (widening) of blood vessels via production of nitric oxide gas, when combined with B vitamins (B6, B9 folic acid and B12), is superior to L-arginine alone at restoring normal endothelial function among patients with high blood pressure.
Among hypertensive patients taking medications, folic acid supplementation has been shown to reduce undesirably high homocysteine levels by 25%, reduce blood pressure and lower the risk for strokes by 12.9% compared to hypertensive patients not taking a folic acid supplement.
Hypertension often occurs among those individuals who are obese or diabetic. A common finding in these disorders is endothelial dysfunction. Endothelial cells line the inside of arteries and control blood pressure by the production of a transient gas called nitric oxide that widens (dilates) or constricts blood vessels to control blood pressure when under physical exertion or mental stress. Zinc is necessary to avert this problem among individuals with diabesity.
A completely zinc-free diet induces hypertension in lab animals.
In another telling study published in the International Journal of Pharmacology, laboratory rats were loaded with sodium, half of them given supplemental zinc in addition to sodium. The sodium-supplied animals developed high blood pressure but the salt + zinc animals did not. Supplemental zinc also prevented a decline in potassium. Sodium fortified animals also gained weight but this was countered by zinc.
Yet another animal study published in the FASEB Journal compared zinc deficient with zinc adequate animals. Blood pressure levels among zinc-deficient animals were highest and zinc-adequate were lowest. Red blood cells were very sticky among zinc deficient animals.
Back in 1995 a report published in the American Journal of Hypertension attempted to answer that question. An ACE (angiotensin-converting enzyme) inhibitor, a beta blocker and a calcium blocker were employed in 30 human subjects with normal blood pressure and 30 subjects with mild to moderate high blood pressure. After 3 months there was a significant decline in blood serum zinc levels regardless of which drug was employed. Magnesium levels also declined.
Does a shortage of zinc translate into hypertension in humans like it does in animals? In another instructive but overlooked study published in 1997, an antioxidant regimen consisting of zinc sulfate (200 mg), vitamin C (500 mg), vitamin E (600 mg) and beta carotene (30 mg) increased availability of nitric oxide and this antioxidant combination was posed as “antihypertensive therapy.”
Magnesium is an important companion with zinc. A concomitant increase in salt consumption and reduction in magnesium intake is associated with increased blood pressure.
Here is the recorded effect of zinc supplementation on the systolic blood pressure of laboratory animals. Also notice the effect upon the immune system (white blood cells):
| Groups |
Systolic blood pressure |
White blood cells |
|
| A | Control animals |
118 |
8,575 |
| B | Zinc-fed animals |
120 |
12,000 |
| C | Salt-loaded |
145 |
10,975 |
| D | Salt-loaded + zinc-fed |
121 |
13,131 |
Researchers concluded salt loading increased arterial blood pressure and zinc supplementation prevented this salt-induced elevation. As sodium blood levels increase, potassium levels declined. Zinc supplementation stabilized potassium levels. Of note, the difference in the blood plasma levels of the four groups listed above was not significant.
Smokers are at greater risk for hypertension. At least one reason why has been explained. Minerals balance out each other: calcium/magnesium, sodium/potassium, zinc/copper. Smoking tobacco is a primary risk factor for hypertension. Tobacco delivers potentially toxic heavy metals (cadmium, nickel and lead). These toxic heavy metals are delivered directly to the lungs as smokers inhale. When levels of cadmium, lead and nickel are higher and zinc is lower, there is the threat of hypertension.
Certainly mental stress would increase blood pressure by activation of adrenal stress hormones that increase heart rate. There are individuals who are anxious and are hypertensive. Anxiety is linked to relatively high copper/low zinc blood plasma levels. The provision of supplemental zinc has been shown to relieve anxiety in patients plagued by this sometimes chronic problem.
A shortage of zinc can emanate for a variety of reasons, making it difficult to know how to take corrective action:
Excess or unbound iron is another deleterious factor in hypertension.
High ferritin (iron storage) levels are an early predictor of hypertension.
High iron stores (iron bound to ferritin) promote atherosclerosis. Iron overloaded patients avert atherosclerosis due to low levels of hepcidin in white blood cells (macrophages). Hepcidin is an iron-regulating hormone.
The effect of zinc supplementation (26.4 mg zinc/day) was reported among two female college students. Over the 4-month period of the study, blood serum ferritin (iron storage) levels fell in both subjects and thyroid hormone levels improved.
In another study when young women were given iron supplements (37 mg/day) it was noted they experienced a decline in their blood plasma zinc levels.
In a study of men with hypertension, 21% had high iron storage (ferritin) levels versus 0% among healthy control subjects used for comparison. Increased iron stores are a feature of hypertension among males. Premenopausal females are not iron overloaded due to monthly menstrual blood losses, red blood cells being the major source of iron within hemoglobin.
Researchers note that ferritin (iron storage) is the 2nd strongest determinant of blood sugar and the 3rd strongest determinant of serum insulin. Ferritin is also a strong determinant of diastolic blood pressure.
While blood serum iron levels and blood iron transport (transferrin) are not associated with ischemic stroke in males, serum ferritin is associated with ischemic stroke in postmenopausal females. Serum ferritin has been associated with increased systolic (greater than 160) blood pressure in women with diabetes and in men with increased (greater than 95) diastolic blood pressure.
High ferritin levels can sometimes be misleading because the body stores iron within the ferritin protein in states of chronic infection and malignancy to withhold iron from feeding these adverse conditions.
Blood serum ferritin levels, but not serum iron, is a significant predictor of hypertension. In fact, rising serum ferritin levels correlate with higher proportions of people with diabetes, coronary artery disease and hypertension.
According to the Iron Disorders Institute, the healthy range for ferritin is 25-75.
For adults who have difficulty lowering their ferritin levels, the provision of supplemental zinc (34 mg/day) has been found to reduce ferritin levels among patients on hemodialysis.
Red meat provides a highly absorbable form of iron (heme iron). It would be wise for hypertensive individuals to limit red meat intake.
Another horrific revelation is that zinc deficiency in the growth years of life may predetermine vulnerability to develop hypertension later in life.
It is not surprising to learn that low maternal zinc levels are associated with hypertension during pregnancy.
In 2006 researchers hypothesized that zinc supplementation would prevent or delay the development of salt-induced hypertension and advocated zinc supplementation in children of hypertensives to prevent the problem among these prone individuals.
When young laboratory rats were broken into two groups, one group fed a moderately zinc deficient diet and the other a mega-dose zinc diet, the zinc-deficient group exhibited impaired ability to generate nitric oxide, the transient gas that dilates arteries. That group of animals was more likely to be hypertensive in adulthood.
It is common in infants and growing children to prefer foods that are not good sources of zinc. Pregnant women may also have marginally zinc-adequate diets. Zinc is essential in the activation of over 300 enzymes, one being nitric oxide synthase, the enzyme responsible for synthesis of nitric oxide and the derivation of citrulline from arginine, amino acids responsible for generating nitric oxide. Chronic shortages of zinc inhibit nitric oxide synthase and produce elevated blood pressure in all mammalian species.
If what has been demonstrated in the animal lab applies to humans, “moderate zinc deficiency in youth may be a risk factor for hypertension in adult life,” say researchers.
Zinc is desirable because it does not lower pressure among individuals with normal blood pressure.
Zinc deficiency impairs the cell receptors responsible for dilatation of blood vessels. The connection between a shortage of zinc and hypertension appears obvious.
However, in 2016 European researchers wrote in the Journal of Hypertension: “the data on the association between serum zinc and hypertension are sparse (and) inconsistent… to date, no prospective evaluation of the association between serum concentrations of zinc and the development of hypertension has been published.”
These researchers conducted their own study of 1652 adults with a known history of hypertension over a 24.7-year time span. Among these subjects, 259 developed hypertension. After adjustments, there was no association demonstrated between zinc intake and hypertension.
A study of obese Korean women found dietary zinc intake (but not zinc blood levels) is associated with reduction of systolic blood pressure.
In a landmark animal study, published in 2012, hypertension was induced with a high-salt diet and then the diet of these animals was supplemented with zinc, manganese and copper. A combination of these minerals was more effective than any single antioxidant mineral in control of blood pressure.
The blood pressure control exerted by this mineral combination was attributed to the reduction of superoxide (an oxygen free radical) via activation of superoxide dismutase (SOD) that negates the production of nitric oxide, a transient gas released in arteries that dilates (widens) blood vessels and therefore control elevated blood pressure.
Another biological action was reduction of an enzyme (NADPH oxidase). In animal studies, NADPH oxidase enzyme is the major source of excess superoxide radical that impairs dilation of arteries.
Researchers concluded: (their study) “confirms the report that zinc supplementation lowers the blood pressure of salt-loaded hypertensive rats.”
Examine the bar chart below that reveals the measure of blood pressure reduction with minerals (% reduction in BP). Group III is salt loaded; group IV is salt-loaded + manganese. Group V is salt-loaded + zinc; Group VI is salt-loaded + 3 minerals. This suggests a multivitamin with these minerals may help maintain blood pressure within the normal range.
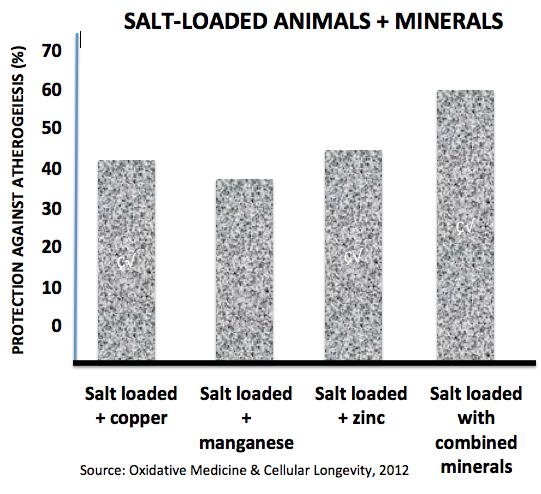
In a telling laboratory experiment, rats were fed a high sodium (salt) diet for 5 weeks to induce high blood pressure and then consumed a trio of minerals (zinc, manganese, copper) that are co-factors in internal enzymatic antioxidants (catalase, glutathione, superoxide dismutase). The mineral-supplemented animals experienced a dramatic 47% decline in blood pressure.
In a landmark animal study published in Oxidative Medicine & Cellular Longevity, salt-loaded lab rats gained weight as fluid volume increased and also experienced a rise in blood glucose levels, insulin and insulin resistance. Provision of the mineral trio reduced weight of these animals. Zinc alone reduced resting (diastolic) blood pressure by 20.68%. The mineral trio protected against atherosclerosis (buildup of plaque inside arteries) by 60.79%, far better than any single mineral. Catalase, glutathione and SOD activity increased and therefore prevented elevation of blood pressure.
This study is very instructive as it points away from the current use of synthetic drugs towards less problematic and economical mineral therapy.
The mineral trio not only normalized blood pressure but improved insulin resistance and significantly lowered blood lipids (triglycerides, LDL cholesterol and atherosclerosis. In other words, what is modern medicine using statin drugs for when the problem of elevated cholesterol originates from a shortage of mineral-generated antioxidant
There is a blood pressure equalizer. In the face of zinc deficiency, adequacy of other minerals can negate the blood pressure elevating effect of low zinc. Over 20 years ago it was reported that where there is higher consumption of calcium, potassium and magnesium, the simultaneous ingestion of sodium is not associated with elevated blood pressure. The conundrum that arises is that the lowest blood pressure readings are reported in human populations where sodium intake is high. It is believed adequate intake of other minerals negates the adverse effects of salt intake. Hard-water areas of the U.S. may be protective against hypertension.
Reduced intake of magnesium is also associated with salt craving.
Mineral-rich bottled water may help avert fructose-induced metabolic issues including hypertension. Brands of magnesium-rich and mineral-rich bottled water are available.
Zinc has to be one of the best-kept secrets that props up over-reliance upon doctoring and prescription drugs. Should the American population ever achieve zinc adequacy, it would be the end of modern medicine as we know it.
In recent times this author has written authoritative reports linking zinc deficiency to atrial fibrillation, dyslexia in school children, arterial disease leading to heart failure, weakened immunity (impaired T-cell activation) that leads to cancer, and overreliance upon vaccines. Modern medicine relies on the perpetuation of widespread zinc deficiency to ensure it has plenty of disease to treat. Sadly, the American population is being gamed.
According to the data presented in this report, zinc, magnesium, manganese, selenium, vitamin B6, folic acid and vitamin E have been identified as important nutritional factors in the control of hypertension.
While correction of diminished taste acuity that leads to unconscious salt craving can be accomplished with zinc supplementation, vitamin A and magnesium have also been identified as nutrients that correct for loss of taste in foods.
A strong rationale could also be made for copper-free multivitamins.
A properly measured supply of these nutrients can best be acquired in a well-designed multivitamin. ©2017 Bill Sardi, Knowledge of Health, Inc.
Posted in Uncategorized ; No Comments »
11
17
52
95
14
24
237
6
56
43
10
116
15
66
105